Circumcision - Physical Problems
These are more than twice as frequent in uncircumcised boys [Fussell et al., 1988].
Phimosis:
Phimosis (‘to tie with a string’ [Remondino, 1891]) is generally regarded as narrowing of the foreskin orifice so as to prevent retraction of the foreskin over the glans. It may arise from physiological adhesion of the foreskin to the glans or to fibrous adhesions. It consists of a permanent preputial constriction often to a pinpoint [Schoen, 2007e]. Trapped secretions and build-up of smegma predispose to poor hygiene, local infections, later penile cancer, and painful erections [Schoen, 2007e]. Severe phimosis may lead to urinary tract infections, localized skin infections, pain when passing urine, retention of urine, kidney stones, and sexual dysfunction [Micali et al., 2006]. Phimosis, if not acted upon early could require intensive penile plastic surgery in the future.
Phimosis is normal in very young boys, but is gone by age 3 in up to 90%. If still present after age 6 it is regarded as a problem. Phimosis affects at least 10% of uncircumcised males, the reported rates being: 20%, as seen by Gairdner in 5–13 year-olds [Gairdner, 1949], 8% at age 8 in Danish boys [Oster, 1968], 9% in New York [Velazquez et al., 2003], 14% in British soldiers [Osmond, 1953], and 9% in German youths [Saitmacher, 1960] and men [Schoeberlein, 1966]. Amongst 15,109 males aged 3-23 in 4 areas of China phimosis was present in 12% [Ben et al., 2008]. Although a rate of 50% in men in Japan [Ohjimi & Ohjimi, 1981] and Bali [Boon et al., 1989] has been reported, a more recent study found that by age 11-15, 77% had a retractable prepuce, i.e., rate of phimosis was 23% [Ishikawa & Kawakita, 2004]. Amongst 13 year-old Japanese boys the incidence of phimosis was 16% [Kayaba et al., 1996]. A report in 2009 involving 10,421 boys aged 0 to 18 years found rate of phimosis to be 99.7% in neonates (age below 28 days), 84% in infants (age 1-12 months), 48% in toddlers (age 1-2), 27% in preschool boys (age 3-6), 12% in schoolboys (age 7-10), 7% in adolescents (age 11-18) [Yang et al., 2009]. Partial phimosis was seen in 0.3%, 16%. 32%, 27%, 20% and 9% in each respective age group. Adhesions were apparent in 0%, 1.3%, 18%, 25%, 29% and 25%, respectively, in each age group. A foreskin that could be retracted normally was apparent in 0%, 0.7%, 2.1%, 11%, 24% and 42%. The circumcision rate was 0%, 0%, 0%, 10%, 15% and 17%. Of all of these children, 13% had undergone forced foreskin dilation in the past, 77% of these forced retractions having been performed prior to school age. Despite having had this procedure carried out, in 13% the phimosis persisted and most of these had scar tissue on the distal foreskin. In Cuba, the foreskin was non retractile in 63%, and completely retractile in only 3.7% [Concepción et al., 2008]. In adolescents (11 to 16 years) 0.9% had phimosis and 81% had a completely retractile foreskin. Of those who had been subjected to forced dilation in the past, 43% had a foreskin that could not be tratracted normally. These had therefore acquired new balanopreputial adhesions subsequently.
In Taiwan the rate of phimosis in one study was 17% in first-grade boys (age 7), 10% in fourth-grade boys (age 10), and 1.2% in seventh-grade boys (age 13), although many more had partial phimosis [Hsieh et al., 2006]. In a different study of boys in the same school years and ages, 0.3% of 13 year-old Taiwanese boys had phimosis [Ko et al., 2007]. Incidence of circumcision was 7% at age 10, and 9% at age 13 in these studies. In an earlier study, however, the rate of phimosis in 10-13 year-old boys was 37% [Su & Yin, 2001].
Balanitis xerotica obliterans (BXO) is the most common cause of pathological phimosis requiring circumcision [Kiss et al., 2005]. This pathological condition causes secondary cicatrization of the foreskin orifice and thus phimosis. The median age for presentation of BXO-induced phimosis is 8-10 years old [Kiss et al., 2005]. Once thought to be rare and a disorder presenting in adulthood, BXO is now regarded as common in young boys, in whom treatment by circumcision is advocated to prevent the complications that occur later in life [Yardley et al., 2007]. Thus whereas a rate of 1% has been reported [Rickwood et al., 2000], others find an incidence in the UK of 5 and 6% in uncircumcised boys under 18 and under 15, respectively [Griffiths & Frank, 1992; Huntley et al., 2003]. A study in Plymouth found BXO in the foreskin specimens of 35% of the 80% of boys aged 3 months to 16 years (mean 6) who had been circumcised following foreskin problems [Yardley et al., 2007]. Histological abnormalities were seen in 85% of those circumcised, chronic inflammation was seen in 47%, and fibrosis was noted in 3% [Yardley et al., 2007]. In this study, overall BXO frequency in the boys referred was 12%. Similarly, a prospective study involving 1,178 boys in Budapest who presented consecutively over the decade 1991-2001 and were then treated by circumcision found by histological examination that BXO incidence was 40%, peaking at age 9-11 (76%), BXO being the cause of the secondary phimosis in all of these [Kiss et al., 2005]. In the study as a whole, 19% of boys had early, 60% intermediate and 21% late form of BXO. A Dutch study in which pathology was performed on all pediatric patients that underwent a circumcision found BXO in 27% [Bochove-Overgaauw et al., 2009]. It noted that clinical findings under-estimate BXO by almost 50%, so that diagnosis must be made based on biopsy. BXO can lead to obstructive renal impairment, as seen in a case report of a 13 year-old boy in Sydney [Sandler et al., 2008]. Circumcision was advocated as the definitive treatment for both early and advanced BXO [Sandler et al., 2008]. Even after treatment risk of penile cancer later in life remains [Sandler et al., 2008]. That is why there is a place for routine biopsy of the foreskin after circumcision for pathological phimosis [Bochove-Overgaauw et al., 2009].
Here is a summary of the literature on prevalence of BXO: 62% (Hungary; 76/123) [Nyirady et al., 2006], 40% (Hungary; 471/1178) [Kiss et al., 2005], 39% (Italy; 45/115) [Mattioli et al., 2002], 37% (Italy; 26/71) [Rossi et al., 2007], 34% (UK; 49/143) [Yardley et al., 2007], 33% (France; 14/43) [Aynaud et al., 1999], 27% (USA; 11/41) [Gargollo et al., 2005], 19% (Denmark; 15/78) [Clemmensen et al., 1988], 14% (UK; 14/100) [Chalmers et al., 1984], 11% (Greece; 8/75) [Liatsikos et al., 1997], 10% (Switzerland; 10/100) [Meuli et al., 1994], 6% (UK; 6/100) [Huntley et al., 2003], 3% (Turkey; 1/32) [Tokgoz et al., 2005].
The narrow foreskin opening causes urinary obstruction that can be partial or complete. As well as urethral stenosis, meatal stenosis is seen, making it a significant condition [Yardley et al., 2007]. Indeed, BXO is generally regarded as an indication for circumcision [Yardley et al., 2007]. In one series in Boston of pediatric BXO, amongst 41 patients, 52% had been referred for phimosis, 13% for balanitis and 10% for buried penis [Gargollo et al., 2005]. Of these, 46% underwent curative circumcision, 27% also had BXO involvement of the meatus and had not only circumcision, but meatotomy or meatoplasty, and 22% required extensive plastic surgery of the penis, including buccal mucosa grafts, demonstrating a more severe and morbid clinical course.
A study in the UK of 100 men aged 17 to 82 (mean 38 years) noted that 31% had a lifelong history of phimosis and 69% had a history of acquired phimosis [Bromage et al., 2007]. Of the men with acquired phimosis, 32% had diabetes [Bromage et al., 2007]. Phimosis may be a warning sign of diabetes, since 12% of the men with phimosis and who had no previous history of a disorder of glucose metabolism or diabetes were found to have diabetes (8%) or impaired fasting glycemia (4%), i.e., prevalence was much higher than the UK average for diabetes of 3.6% [Forouhi et al., 2006]. Balanitis is common in diabetes (see section on inflammatory dermatoses) and recurrent infection and scarring is probably responsible for the phimosis that develops.
Phimosis also increases risk of penile cancer (discussed later) and treatment by complete circumcision to prevent this outcome is advocated.
The definitive treatment for phimosis is circumcision, which then also provides the many other benefits conferred by this simple procedure. In India preputial adhesions were responsible for most 'physiological' phimosis and one to eight adhesiolysis sessions removed these in 95% of the children affected (mean age 22 months) [Kumar et al., 2009].
Phimosis can be treated with topical steroid creams, but these need to be applied for at least a month, have a fairly low to moderate success rate, can lead to iatrogenic Cushing's syndrome, adrenal suppression, delayed growth, skin atrophy, and of course offer no benefit in prevention of other conditions associated with having a foreskin [Lund et al., 2005; Yang et al., 2005; Zampieri et al., 2005; Ku et al., 2007; Pileggi & Vicente, 2007; Esposito et al., 2008; Palmer & Palmer, 2008; Singh & Bunker, 2008; Ghysel et al., 2009; Letendre et al., 2009]. A randomized controlled trial showed that although steroid creams may be effective in the short term, in the long-term, recurrence of phimosis is frequent, requiring retreatment or circumcision [Letendre et al., 2009].
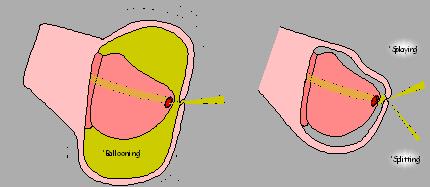
Ballooning: See diagram below:
Paraphimosis: This is when the retracted foreskin cannot be brought back again over the glans and is a very painful problem. Backward pressure to the kidney may impede its function and have cardiovascular consequences. It is relieved by circumcision or slitting the dorsal surface of the foreskin.
The foreskin problems referred to above also mean intercourse is painful.
Pearly penile papules: These have been seen in 42% of uncircumcised, but less so (26%) in circumcised, UK men aged under 25 (P < 0.05) [Agha et al., 2009]. The frequency in older men was 11%.
Zipper injury: In uncircumcised boys the foreskin can become accidentally entrapped in zippers, resulting in pain, trauma, swelling and scarring of this appendage. Foreskin accidents in men can also occur.
Elderly men:
In elderly men, infections and pain from balanoposthitis (see below), phimosis and paraphimosis are seen and carers report problems in achieving optimal hygiene in uncircumcised men. The need for an appliance for urinary drainage in quadraplegics and in senile men is facilitated if they are circumcised. Nursing home staff have particular difficulty performing their duty of washing the genital area of uncircumcised elderly men, particularly with the onset of dementia. Such men can react violently towards staff or family during attempts to wash under the foreskin. This is an under-recognized problem and far from the mind of a parent or neonatologist when considering circumcision for an infant, so that information on the gerontological perspective should also be given at birth [Frank, 2000].
Dr. Sam Kunin in Los Angeles points out that "As a urologist with extensive experience with our aging population I have been called to nursing homes on an emergency basis several times for paraphimosis induced when disoriented men have pulled their foreskin back and the nurses could not reduce the paraphimosis. This can cause gangrene of the distal skin and possible damage to the penis itself. It requires immediate emergency intervention." Dr. Kunin also points out that "if the paraphimosis cannot be reduced manually an emergency dorsal slit must be performed."
Another problem he highlights is "inability to catheterize due to a tight foreskin, which becomes worse when the patient cannot wear a condom catheter. In this group of people, local irritation, odor and infection is a serious problem among many uncircumcised males. These problems will only multiply as our aging population continues to grow."
• Paraphimosis induced when disoriented men have pulled their foreskin back and the nurses could not reduce the paraphimosis. This can cause gangrene of the distal skin and possible damage to the penis itself. It requires immediate emergency intervention. If the paraphimosis cannot be reduced manually an emergency dorsal slit must be performed.
• Inability to catheterize due to a tight foreskin, which becomes worse when the patient cannot wear a condom catheter.
• ln this group of people, local irritation, odor and infection is a serious problem among many uncircumcised males. These problems will only multiply as our aging populations continues to grow.”
Bathroom 'splatter': Boys and men who are not circumcised can be a source of irritation if they do not retract the foreskin when they urinate, as 'splatter' will occur. Although not a medical problem, it is a source of annoyance for other people (such as a parent or partner) if it is they who have the job of cleaning the bathroom.
Frenular chordee: This results from an unusually thick and often tight frenulum and prevents the foreskin from fully retracting, being present in a quarter of all uncircumcised males [Griffin & Kroovand, 1990]. The frenulum then tears during intercourse or masturbation. Since scar tissue on the foreskin is generally more fragile and less elastic than normal tissue, the tear often re-occurs causing pain, bleeding and is an impediment to sexual activity. A short frenulum is a common cause for dyspaeunia (painful sexual intercourse) seen in uncircumcised men [Gyftopoulos, 2009]. This problem can be solved by excising the frenulum during a circumcision. Frenoplasty (removing just the tight frenulum) is also possible. One way of doing this is by the “pull and burn” method [Gyftopoulos, 2009].
Psychological sequelae: Follow-up 5 years later of 117 boys circumcised for phimosis, balanitis scarring of the prepuce, or ballooning when urinating found that 95% expressed complete satisfaction and the only psychological effect was slight shyness in the school change-room in 9% of boys in this Swedish study [Stenram et al., 1986b; Stenram et al., 1986a]. The study showed that parents had nothing to fear for their son's psychological well-being from circumcision.