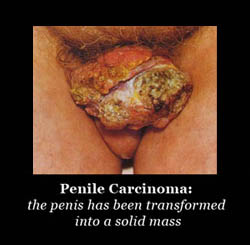
Circumcision - Cancer of the Penis
and HPV Infection
Incidence
The predicted lifetime risk of penile cancer for an uncircumcised man has been estimated as 1 in 600 in the USA and 1 in 900 in Denmark [Kochen & McCurdy, 1980]. Penile cancer accounts for less than 1% of all malignancies in men in the USA and 0.1% of cancer deaths, the 5-year survival rate being approx. 50% [American, 2005a]. Mortality rate is 25-33% [Kochen & McCurdy, 1980; Maden et al., 1993].
The annual incidence of cancer of the penis in the USA is approx. 1 per 100,000 men per year [Crawford et al., 1988; American, 2005a]. (In comparison, cervical cancer incidence is 10 times higher [see below], breast cancer is 60 times higher, prostate cancer is 100 times higher, and fatal heart attack is 200 times higher.) Statistics on the American Cancer Society web page point to 1,280 new cases of penile cancer in 2007, with 290 deaths [American, 2007b]. The incidence of primary malignant penile cancer in the USA from 1973 to 2002 was 0.69 per 100,000, decreasing over the decades from 0.84 to 0.58 per 100,000 [Barnholtz-Sloan et al., 2007]. From 1998 to 2003, 4967 men were diagnosed with invasive squamous cell carcinoma in the USA (less than 1% of all new cancers in men; 0.81 cases per 100,000 men) [Hernandez et al., 2008a]. Squamous cell carcinoma is the most common type of penile cancer in the USA, representing 93% of all malignancies [Goodman et al., 2007].
In the USA, Hispanic men have the highest incidence (6.6 per million), then Black men (4.0 per million), White (3.9), American Indians (2.8) and Asian-Pacific Islanders (2.4) [Goodman et al., 2007]. For ages >85 y incidence was 47 and 36 per million in Hispanic and Black men, respectively [Goodman et al., 2007]. Owing to earlier diagnosis, incidence has been decreasing by 1.9% per year in Blacks and 1.2% in Whites [Goodman et al., 2007]. The majority (61%) were diagnoses at the localized stage. Regional differences were apparent. Another report gives figures for 1993 to 2002 of 1.01 per 100,000 for white Hispanics, 0.77 for Alaskan native/American Indians, 0.62 per 100,000 for Blacks and 0.51 for whites who are not Hispanic [Barnholtz-Sloan et al., 2007]. This correlates inversely with incidence of circumcision between these groups.
Penile cancer is regarded as an "emerging problem" [Micali et al., 2006]. This large review also noted that "public health measures, such as prophylactic use of circumcision, have proven successful" [Micali et al., 2006]. Neonatal circumcision virtually abolishes the risk [Schoen, 1996].
The rate data in the USA has to be viewed in the context of the high proportion of circumcised men in the USA, especially in older age groups, and the age group affected (mean age at presentation = 60 years [Ries et al., 1998]), where older men represent only a portion of the total male population.
Thus the incidence of 1 in 100,000 men per year of life translates to 75 in 100,000 during each man's lifetime (assuming an average life expectancy of 75 years). However, penile cancer occurs almost entirely in uncircumcised men. If we assume that these represent 30% of males in the USA, the chance an uncircumcised man will get it would be (very approximately) 75 per 30,000 = 1 in 400. Perhaps not surprisingly this accords with the incidence that is actually seen (as stated in the first paragraph).
In 5 major series in the USA, starting in 1932 [Wolbarst, 1932], not one man with invasive penile cancer had been circumcised neonatally [Maden et al., 1993], i.e., this disease is almost completely confined to uncircumcised men. In fact penile cancer is so rare in a man who had been circumcised in infancy, that when it does occur it can even be the subject of a published case report [Kanik et al., 1997]. The finite residual risk appears to be greater in those circumcised after the newborn period, but still less than the uncircumcised. In this regard penile cancer in circumcised men (av. age 62) in Saudi Arabia (where circumcision is performed in older children) was associated with ritual, nonclassical, vigorous circumcision [Seyam et al., 2006].
Lifetime risk in the total population of circumcised men is only 1 in 50,000 to 1 in 12,000,000 [Wiswell, 1995; Wiswell, 1997a]. In a study of 213 cases in California only 2 of 89 men with of invasive penile cancer was circumcised in infancy, so that uncircumcised men were stated to have a 22 times higher risk [Schoen et al., 2000b; Schoen et al., 2000c]. Of 118 with the localized, and thus more easily curable, variety of penile cancer, namely carcinoma in situ (which is not lethal), only 16 had been circumcised as newborns, i.e., incidence was 3-fold higher in the uncircumcised [Maden et al., 1993; Schoen et al., 2000b; Schoen et al., 2000c]. A study in Louisiana found that only 2 of 45 penile cancer patients had been circumcised in infancy [Carver et al., 2002]. Circumcision later in life is much less effective [Tsen et al., 2001].
Overall there were 50,000 cases of penile cancer in the USA from 1930 to 1990 and these resulted in 10,000 deaths. Only 10 of these cases were in circumcised men [Schoen, 1991], and these had been circumcised later in life. In Denmark (circumcision rate = 2%), penile cancer has been decreasing steadily [Frisch et al., 1995] in parallel with an increase in indoor bathrooms. Urban unmarried men were more likely to get it.
Since the rate of penile cancer in Denmark is lower than in the USA other factors besides circumcision are also at work in these climatically, genetically, dietarily and culturally different countries. The statistics for Denmark have been used by anti-circumcision advocates to draw a sweeping and fallacious conclusion about lack of circumcision per se in penile cancer. The Danish themselves have concluded that although their uncircumcised men are at lower risk, this is only 1 in 900 as opposed to 1 in 600 in the USA, as stated above [Kochen & McCurdy, 1980]. A study in Spain concluded that "circumcision should be performed in childhood [as a] prophylactic [to penile cancer]" [Sanchez Merino et al., 2000].
As a historical point of interest, Diego Rivera, the famous Mexican muralist, who had multiple sexual partners over many years in a country where most men are uncircumcised, developed penile cancer [Schoen, 2007d]. He refused penectomy (surgical removal of the penis) and instead (as a Communist) went to the Soviet Union for radiation therapy. He died a painful death from the disease and the side effects of his therapy.
In underdeveloped countries the incidence is higher: approx. 3-10 cases per 100,000 per year [Kochen & McCurdy, 1980]. In those underdeveloped countries where circumcision is not practiced routinely, such as South America and parts of Africa, it can be ten times more common than in developed countries, representing 10-22% of all male cancers [Narayana et al., 1982; Gross & Pfister, 2004; American, 2005a]. In Uganda and some other African countries it is the most common malignancy in males, leading to calls for greater circumcision [Dodge & Linsell, 1963]. Enormous differences are, moreover, seen amongst third world nations according to circumcision rates. As well as Uganda, Puerto Rico [World., 1997], India and Brazil [Villa & Lopez, 1986; Favorito et al., 2008] most men are uncircumcised and penile cancer is very common. Brazil has one of the highest rates of penile cancer - 3-7 per 100,000 inhabitants, i.e., 6-14 per 100,000 males, comprising 2-6% of all male neoplasias, with 7% being seen in men aged less than 35 and 39% in men older than 66 [Favorito et al., 2008]. The uncircumcised made up 87% of cases. All tumors seen in men circumcised in childhood were low-grade, whereas 12% of those circumcised in adulthood had high-grade tumors [Favorito et al., 2008].
In Australia there were 67 cases in 2003, and over the decade to that year cases averaged 66 per year [Australian, 2004b]. Typical age distribution of cases is approx. 4% aged in their 30s, 14% in their 40s, 15% in their 50s, 22% in their 60s, 31% in their 70s, and was 12% in those aged over 80 [Australian, 2004a]. One in four died as a result, the rate being higher in older men. The annual incidence of penile cancer is 0.8 per 100,000 population [Australian, 2004a], i.e., was similar to the USA, and was also similar in each state of Australia. Life-time (age 0–74) risk was estimated as 1 in 1,574 males [Australian, 2004a]. As in the USA, over two-thirds of older men in Australia are circumcised, so any future decline in proportion of uncircumcised males in the Australian population will, by itself, be expected to be accompanied by an escalation in the rate of penile cancer.
As mentioned earlier, the rate of cervical cancer is, in contrast, 10 times higher, with 725 cases in Australia in 2003 (incidence 9.1 per 100,000) and 212 deaths [Australian, 2007].
In Israel, where almost all males are circumcised, the rate of penile cancer is extremely low: 0.1 per 100,000, i.e., is 1/10th that of Denmark [World., 1997; Solsona et al., 2004].
Cause: Role for human papillomavirus (HPV) infection
Cancer of the penis presents as carcinoma in situ or invasive penile cancer. The proportion of each of these is roughly equal (45% vs 55% in the USA). Invasive penile cancer is lethal, whereas carcinoma in situ is comparatively benign. Moreover, the former is not necessarily a continuum of the latter [Daling et al., 2005].
Human papillomavirus (HPV) is present in most basaloid and warty carcinomas which comprise 50% of cases [Gross & Pfister, 2004]. Similarly, in women, half of all vulvar carcinomas are HPV-positive (cf. the close to 100% positivity for high-risk HPVs in cervical cancer). High-risk HPV is found more frequently in verrucous carcinomas than giant condylomas (which are caused by low-risk HPV). Although relatively harmless, such benign condylomas are readily apparent and, as shown in the picture below of a promiscuous man who was still having sex at the time, can be quite shocking to look at.
 |
 |
Keratinizing and verrucous carcinomas are HPV positive in one-third of cases [Gross & Pfister, 2004]. A Spanish study found HPV in 78% of penile carcinoma specimens and of these 84% had HPV16 and 11% had HPV18 [Pascual et al., 2007]. A Danish study found 65% of squamous cell carcinomas had HPV, with 92% of these being HPV16 [Madsen et al., 2008]. A study in Thailand found HPV in 82% of penile cancers, of which 55% had HPV18, followed by HPV6 (43%), with a large proportion having each [Senba et al., 2006].
Thus high risk HPV (types 16, 18 and a large number of rarer types) are found in a large proportion of cases and there is good reason to suspect that they are involved in the causation of penile cancer [McCance et al., 1986], i.e, are the same viral types as are responsible for virtually all cases of cervical cancer in women (see below).
HPVs, notably high-risk types, are more common in uncircumcised males [Niku et al., 1995; Kohn et al., 1999; Castellsague et al., 2002; Baldwin et al., 2004; Lajous et al., 2005]. In Copenhagen, Denmark, being uncircumcised was associated with a 5-fold higher likelihood of being infected with HPV [Svare et al., 2002].
In a large study published in the prestigious New England Journal of Medicine in 2002 HPV was detected in 19.6% of 847 uncircumcised men, but only 5.5% of 292 circumcised men (overall odds ratio after adjusting for potential confounding factors = 0.37) [Castellsague et al., 2002]. In this study, sampling was of the urethra and glans penis/coronal sulcus. Amongst men attending vasectomy clinics in Mexico, HPV was 5 times lower in those who were circumcised [Vaccarella et al., 2006]. In a study of healthy military men in Mexico the odds ratio for persistent HPV infection was 10 times higher in uncircumcised compared with circumcised [Lajous et al., 2005].
The high-risk types of HPV produce flat warts that are normally only visible by application of dilute acetic acid (vinegar) to the penis. The majority of infections are subclinical, being more prevalent in uncircumcised men with balanoposthitis [Kohn et al., 1999]. The data on high-risk HPVs should not be confused with the incidence figures for genital warts, which are large and readily visible, and are caused by the relatively benign HPV types 6 and 11 [Katelaris et al., 1988].
Distribution on penis:
The distribution of HPV types on the penis appears to be important, there being a much higher prevalence of high-risk types with proximity to the tip of the penis. In one study the distribution of HPV on the penis was reported as 28% foreskin, 24% shaft, 17% scrotum, 16% glans and 6% urine [Weaver et al., 2004]. In the HIM study, involving men in the USA, Mexico and Brazil, high-risk HPV types were lower in circumcised men (OR 0.70) as were low-risk HPV types (OR 0.63) [Giuliano et al., 2009]. HPV prevalence ranged from 41% on the shaft to 4.7% in se men [Nielson et al., 2009]. In the HIM study, the strength of the association between circumcision and reduced HPV decreased with distance from the prepuce/urethra. The adjusted OR was 0.17 for the urethra, 0.44 for the glans/corona, 0.53 for the shaft, and no difference for scrotum, peri-anal area, anal canal and se men [Nielson et al., 2009]. A study in Hawaii of primarily heterosexual men found HPV infection of the glans/coronal sulcus was almost twice as high in uncircumcised men (46%) compared with circumcised men (29%) [Hernandez et al., 2008b]. This study also found that uncircumcised men had a higher risk of oncogenic HPV types (adjusted OR 2.51) and infection with multiple HPV types (adjusted OR 3.56). In uncircumcised men, HPV prevalence on the foreskin (44%) was comparable to that on the glans/corona. In Kisumu, Kenya, high-risk HPV in 2,705 uncircumcised men aged 17-28 was 31.2% glans and 12.3% shaft (P<0.0001) [Smith et al., 2009]. Testing was done in Amsterdam using PCR. HPV16 was the most common type, with 29% infected with more than one type. Not surprisingly, men with HPV were also more likely to have other STIs. Genital warts were uncommon (1%).
Circumcised men clear HPV faster:
Although HPV seroprevalence was similar for circumcised and uncircumcised men in a New Zealand study [Dickson et al., 2009], a study in Tuscon, Arizona, of 285 men aged 18-44 found that circumcised men clear penile oncogenic (but not non-oncogenic) HPV infections 6 times faster than uncircumcised men [Lu et al., 2009]. A strength of each of these studies was that they had a longitudinal design. The ability of circumcised men to clear high-risk HPV faster would further explain their lower risk of penile cancer, and of cervical cancer in their partner(s). Moreover, as mentioned above, in healthy Mexican military men, OR for persistent HPV infection was 10-times higher in those who were not circumcised [Lajous et al., 2005]. Interestingly, men who had had 16 or more lifetime sex partners were 4.9 times more likely to clear oncogenic HPV infection [Lu et al., 2009].
Meta-analyses:
A meta-analysis of 8 studies was published in 2007. This showed that circumcision was associated with a statistically significant reduced risk of penile HPV and related lesions (odds ratio 0.56; 95% CI = 0.39-0.82) [Castellsague et al., 2007]. The meta-analysis by these reputable workers was prompted by the publication at the time of a "biased, inaccurate and misleading meta-analysis" by the notorious anti-circumcision activist, Robert Van Howe, who is well known for using statistical games to discredit and even invert data from good peer-reviewed studies whose conclusions disagree with his biases.
In 2009 another meta-analysis was published. This included data on high-risk HPV types from, 14 studies (5 US, 2 Mexican, 2 Australian and one each from England, Denmark, South Korea, Kenya, and the multination study in 2002 referred to above), and involving 5,880 circumcised and 4,257 uncircumcised men). It found circumcision to be protective, with an OR of 0.52 (95% CI = 0.33-0.82) [Bosch et al., 2009]. The meta-analysis found only a slight reduction in low-risk HPV types (OR 0.89; 95% CI 0.59-1.33). These manifest as visible warts and tend to occur on the shaft of the penis, a site of infection unlikely to be affected by circumcision [Bosch et al., 2009].
Randomized controlled trials:
The protection afforded by circumcision against HPV is now supported by two RCTs. One trial, conducted in Uganda and published in the New England Journal of Medicine, found that at 24 months high-risk HPV in swabs from the coronal sulcus of the penis was present in 18% of the circumcised men compared to 28% of the uncircumcised men, giving an adjusted prevalence ratio of 0.65, i.e., the protective effect of circumcision was 35% [Tobian et al., 2009b]. When confining the analysis to samples positive for beta-globin (meaning cells were present), HPV was found in 14.9% of the circumcised group compared with 26.5% of the uncircumcised group indicative of a 44% protective effect [Tobian et al., 2009b]. Multiple high-risk HPV types were detected in 4.3% of circumcised men and 12.2% of uncircumcised men, indicating a 65% protective effect of circumcision against these [Tobian et al., 2009b]. The prevalence of non-high-risk HPV types was 26% vs 39%, indicating a protective effect of 35% [Tobian et al., 2009b]. In another report from the Rakai trials, among 230 circumcised men, 14% acquired new HPV infections over 24 months, compared to 25% of 267 uncircumcised men, giving an adjusted incidence rate ratio of 0.58, meaning a 42% protective effect [Gray, 2009a]. Circumcised men were, moreover, 65% less likely to be infected by multiple high-risk HPV types.
In a randomized controlled trial in South Africa, high-risk HPV in urethral swabs was 34% lower in the circumcised group at 21 months after surgery [Auvert et al., 2009d]. The authors state, moreover, that owing to the fact that some men would have already been infected with HPV before inclusion in the trial, the true effect of circumcision would have been higher than what they reported. Others have pointed out that HPV detection may have been less than optimal owing to sampling at the urethra rather than the glans, coronal sulcus or shaft, so under-estimating the efficacy of circumcision in relation to HPV prevalence [Auvert et al., 2009b; Gray et al., 2009c].
PIN and CIN:
Interestingly, 93% of men whose female partner was positive for early signs of cervical cancer (cervical intra-epithelial neoplasia, CIN) had the male equivalent, penile intra-epithelial neoplasia (PIN) [Aynaud et al., 1994]. This reflects the fact that the disease, via HPV, is sexually transmitted. Oncogenic HPV was present in 75% of patients with PIN grade I, 93% with PIN grade II and 100% of PIN grade III, which is one step before penile cancer itself [Aynaud et al., 1994]. Moreover, the rate of PIN was 10% in uncircumcised men compared with only 6% in circumcised men [Aynaud et al., 1994]. HPV DNA was found in 80% of tumor specimens, with 69% being the high-risk type 16 [Daling et al., 2005]. That condom use may lower HPV infection was reported in a study of 393 men in Tucson, Arizona [Baldwin et al., 2004]. In another, of 463 men in Tucson and Tampa, condom use halved the prevalence of oncogenic HPV [Nielson et al., 2007]. It is important to note that condom use did NOT eliminate HPV infection - far from it!
Phimosis:
Phimosis is strongly associated with invasive penile carcinoma (adjusted odds ratio = 16 in one study [Tsen et al., 2001] and 11 in another [Daling et al., 2005]). In fact 45-85% of men with penile cancer have a history of phimosis [Dillner et al., 2000; Tsen et al., 2001; Favorito et al., 2008]. Phimosis causes dysplastic (cancerous) changes in the skin of the preputial sac [Reddy et al., 1984]. Although length of the foreskin has been suggested as a factor, the evidence for this is weak [Velazquez et al., 2003]. In this study 52% of penile cancer cases with a long foreskin had phimosis. Phimosis is associated with a 12.1-fold (95% CI 5.57-26.2) increase in risk of penile cancer [Morris et al., 2011a].
Smegma:
Smegma (found only under the foreskin) was implicated in an early study [Pratt-Thomas et al., 1956]. The carcinogenicity of smegma was subsequently confirmed by others [Dennis et al., 1956; Heins & Dennis, 1958; Reddy & Baruah, 1963]. It is not clear, however, what component was responsible, and could have been HPV present in the smegma. Smegma may cause chronic inflammation and recurrent infections that lead to preputial adhesions and phimosis [Reddy et al., 1984; Tsen et al., 2001]. Male horses produce large amounts of smegma and 23% of cancers in these animals involve the penis. Geldings do not get erections that would normally help eliminate smegma, and in such horses penile cancer is 10 times higher than in stallions [Schoeberlein, 1966]. Add at end: A meta-analysis found that smegma is associated with a 3.04-fold (95% CI 1.29-7.16) increase in risk of penile cancer [Morris et al., 2011a].
Balanitis, lichen sclerosis, herpes and other factors:
Chronic relapsing balanitis of bacterial, mycotic or viral origin may also increase risk of invasive penile cancer [Haneke, 1982; Sayed et al., 1993]. A history of balanitis has been reported in 45% of penile cancer patients compared with 8% of controls [Dillner et al., 2000; Schoen et al., 2000b]. A meta-analysis found that balanitis is associated with a 3.82-fold (1.61-9.06) increase in risk of penile cancer [Morris et al., 2011a]. Penile lichen sclerosis (balanitis xerotica obliterans (BXO)), an inflammatory disorder that can lead to meatal stenosis or phimosis is associated with penile cancer (reviewed in [Micali et al., 2006]). Incidence in penile carcinoma patients was initially estimated as 2.6-5.8%, but subsequent research found the rate of BXO to be very much higher. In one study it was 28%, where 77% of patients had squamous cell carcinoma and 23% carcinoma in situ [Pietrzak et al., 2006]. Other studies found BXO in 33% [Velazquez & Cubilla, 2003], 44% [Perceau et al., 2003] and 50% [Powell et al., 2001] of cases of squamous cell carcinoma. The rate of HPV infection was 2.6 times higher amongst patients with penile lichen sclerosis [Nasca et al., 2006]. Lichen sclerosis is not always associated with presence of HPV and it could be that lichen sclerosis acts as a catalyst in the onset of penile cancer [Ranjan & Singh, 2008].
Although this and other evidence that found oncogenic HPV to be higher in patients with genital lichen sclerosis (17% vs 9%), other data has suggested that lichen sclerosis is a preneoplastic condition unrelated to HPV infection (reviewed in [Micali et al., 2006]). One review suggested that approximately half of penile squamous cell carcinomas (which represent 95% of penile neoplasms) are associated with lichen sclerosis and half with HPV [Singh & Bunker, 2008].
A co-carcinogenic role of recurrent herpes simplex type 2 (HSV-2) in penile cancer has also been suggested [zur Hausen, 1983; Fernando & Wanas, 1991].
The widely used vaginal spermicide, nonoxynol-9, greatly increases susceptibility of the genital epithelium to HPV16 infection [Roberts et al., 2007]. In this study, carrageenan, a polysaccharide present in some vaginal lubricants, prevented infection.
In addition, other factors, such as smoking (4.5-fold increase in risk [Daling et al., 2005]), poor hygiene (even in the absence of phimosis) and other STIs have been suspected as contributing to penile cancer as well [Maden et al., 1993; Bailis, 2000], but it would seem that lack of circumcision is the primary prerequisite, with such other factors adding to the risk in the uncircumcised man. Indeed, there is no scientific evidence that improved penile hygiene is effective in reducing the risk in an uncircumcised man [Moses et al., 1998]. A study in California showed there was no correlation between penile cancer and frequency of bathing or method of cleaning the anogenital area before or after sexual intercourse [Tsen et al., 2001]. It has been concluded that circumcision in early childhood, by eliminating phimosis, may help prevent penile cancer [Daling et al., 2005].
There may be two routes to penile cancer: one via sexual transmission of oncogenic HPV in young men and the other unrelated to HPV that mostly affects older men (reviewed in [Micali et al., 2006]).
Treatment:
Complete or partial surgical amputation of the penis is the traditional treatment. Radiation is an alternative (or additional) therapy and in early-stage disease can preserve function of the organ. In a retrospective study in Switzerland of 41 consecutive patients with non-metastatic invasive carcinoma of the penis 44% underwent surgery (to remove all or part of the penis, as well as lymph nodes in one third), followed by radiation therapy (in three-quarters) and the rest (56%) had just radiation therapy [Zouhair et al., 2001]. Over the median 70 months of follow-up 63% relapsed. For all patients 5-year survival rate was 57% and 10-year survival was 38%. Local relapse rate was lower in those who underwent surgery. However, there was no difference in survival when compared with radiation therapy, either alone, or in conjunction with salvage surgery. In a Swiss study, local control was better with surgery (87%) than radiation therapy alone (44%), but 5 year survival was similar: 53% vs. 56% [Ozsahin et al., 2006]. After 5 years 43% of those with an intact penis were alive, and by 10 years this was 26%. A recent review has emphasized the role of lack of circumcision and poor prognosis, as well as providing an update on treatment options [Busby & Pettaway, 2005].
The psychosexual implications to a man are, understandably, not inconsequential [Opjordsmoen et al., 1994]. The fact that, as is the case for breast cancer, the sex-related organ is often surgically removed adds to the devastating physical and emotional impact of penile cancer. But the 5-year survival rate is lower [Ries et al., 1998]. It would be cold comfort to a man so afflicted to know that his disease could almost certainly have been prevented had he been circumcised in infancy.
Cost:
Financial considerations are, moreover, not inconsiderable. In the USA it was estimated that the cost for treatment and lost earnings in a man of 50 with cancer, even back in 1980, was $103,000 [Harturian et al., 1980]. A more recent estimate of just the direct (discounted lifetime) medical costs per case was $15,120 [Hu & Goldie, 2008]. This did not include long-term costs and management fees, nor loss of earnings. The total lifetime cost of new cases of penile cancer attributed to HPV16 and 18 (25% of penile cancers) in the USA in 2003 alone was estimated as US$4.4 million [Hu & Goldie, 2008].
Deaths from penile cancer vs. circumcision:
In Australia between 1960 and 1966 there were 78 deaths from cancer of the penis and 2 from circumcision. (Circumcision fatalities today are virtually unknown in hospital and other clincial settings.) At the Peter McCallum Cancer Institute 102 cases of penile cancer were seen between 1954 and 1984, with twice as many in the latter decade compared with the first [Sandeman, 1990]. Moreover, several authors have linked the rising incidence of penile cancer to a decrease in the number of neonatal circumcisions [Dagher et al., 1973; Sandeman, 1990]. It would thus seem that "prevention by circumcision in infancy is the best policy". Indeed it would be an unusual parent who did not want to ensure their child was protected completely by this simple procedure. The protective effect of circumcision against invasive penile cancer is in fact equivalent to the protective effect that not smoking has against lung cancer and heart disease [Schoen, 2007e]
Thus, to quote, "Despite overwhelming evidence from urological surgeons that neoplasm of the penis is a lethal disease that can be prevented by removal of the foreskin, some physicians continue to argue against routine newborn circumcision in a highly emotional and aggressive fashion" [Dagher et al., 1973]. In the interests of public health, such ignorance must be eliminated.



