Circumcision - The Procedure Itself
There is no standard circumcision procedure and the issue of standards has been a rallying call for years. At the Western Section American Urologic meeting in 2007 Dr Sam Kunin, who practices in Los Angeles, compared and contrasted clamps and discussed what he considered should be the minimal standards for circumcision. So here are the most common methods used by doctors.
Circumcision of the neonate:
The newborn period provides a window of opportunity for circumcision [Schoen, 2007b]. The newborn, having recently experienced the considerable trauma of birth, has elevated levels of normal stress-resistance hormones. Babies heal quickly, are resilient, and use of local anesthesia means little or no pain. Since the inner and outer foreskin layers adhere to each other, sutures are rarely needed.

There is no evidence of any long-term psychological harm arising from circumcision. The risk of damage to the penis is extremely rare and avoidable by using a competent, experienced doctor. Unfortunately, because it is such a simple, low-risk procedure, it had once been the practice to assign this job to junior medical staff, with occasional devastating results. Anecdotes of such rare events from the past should be viewed in perspective. Parents or patients nevertheless need to have some re-assurance about the competence of the operator. Also the teaching of circumcision to medical students and practitioners needs to be given greater attention because it is performed so commonly and needs to be done well. A model to teach interns has, moreover, been produced [Erikson, 1999].
Surgical methods often use a procedure that protects the penis during excision of the foreskin. In the USA the most commonly used devices are the GOMCO (GOldstein Medical Company) clamp (67%) invented in 1934, MOGEN clamp (10%) invented in 1945 and PlastiBell (19%) [Stang & Snellman, 1998] invented by Hollister Inc, USA in 1950. Pictures of these can be found in refs [Langer & Coplen, 1998; Alanis & Lucidi, 2004], and the latter in particular discusses the procedure, as well as contraindications.
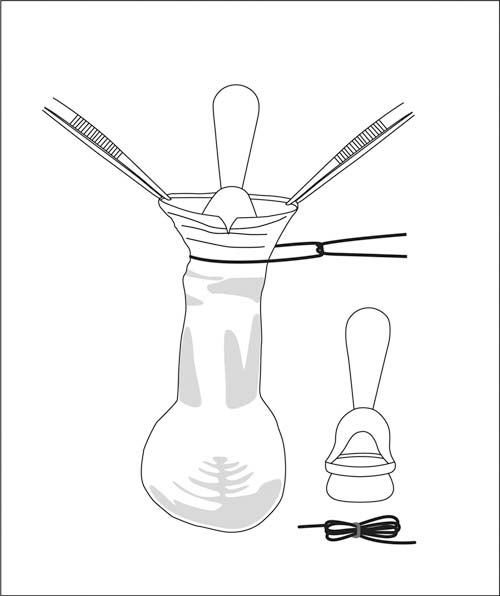
The Plastibell is a clear plastic ring with handle and has a deep groove running circumferentially. (Diagram modified from Elder (2007a).)
Plastibell method:
The Plastibell is a clear plastic ring with handle and has a deep groove running circumferentially (see diagram above). It provides a “no scalpel” circumcision in that the foreskin is not cut off the penis during the procedure. The adhesions between glans and foreskin are divided with a hemastat (artery forceps). Then the foreskin is cut longitudinally starting at the distal end dorsally to allow it to be retracted so that the glans (the head of penis) is exposed [Elder, 2007a]. The Plastibell comes in 6 sizes. The appropriate one is chosen and applied to the head. The ring is then covered over by the foreskin. A ligature is tied firmly around the foreskin, crushing the skin against the groove in the Plastibell. Then the excess skin protruding beyond the ring is trimmed off. Finally, the handle is broken off at the end of the procedure. The entire procedure takes 5 to 10 minutes, depending on the experience and skill of the operator. The compression against the underlying plastic shield causes the foreskin tissue to necrose (die). The ring falls off in 3 to 7 days leaving a circumferential wound that will heal over the following week. Typically, the glans will appear red or yellow until it has cornified. Thus the Plastibell method eliminates the need to actually cut the remnant foreskin off [Gee & Ansell, 1976; Holman et al., 1995].
As described in the next section, all circumcisions should involve adequate anesthesia, using either EMLA cream, dorsal penile nerve block, penile ring block, or a combination of these prior to the operation.
Whatever the method, post-operative care, as advised by the doctor, must be undertaken, usually by the parents. Cosmetic results have met with unanimous parental acceptance [Duncan et al., 2004].
Dr Terry Russell, OAM, in Brisbane, Australia, has developed a simple, pain-free method involving 2 hours EMLA cream with the penis wrapped in cling wrap (done by the parents prior to arrival at the clinic), followed by a modified Plastibell circumcision [Russell & Chaseling, 1996]. The technique is described in detail on his website (www.circumcision.com.au). Dr Russell has used it in over 25,000 circumcisions on boys of all ages from neonate to puberty. Because complete anesthesia is achieved by EMLA cream for 2 hours, Dr Russell reports that no pain is experienced for 5 hours after the Plastibell is applied, meaning the circumcision is completely pain free at all stages. These were all a complete success with no serious or moderate complications, apart from one boy who developed mild methemoglobinemia (from the EMLA cream) that overnight resolved spontaneously with no medical intervention after immediate hospital admission.
Dr Terry Russell
In collaboration with Prof Roger Short, a video (“no scalpel circumcision”) that teaches the Russell method was produced for Botswana, and another, filmed in Vanuatu was produced for use in Papua New Guinea. These were aimed primarily to reduce HIV/AIDS in these countries. Moreover, since the simple plastic Plastibell device is now off patent it can be produced at very low cost to help reduce AIDS in poor countries [Short, 2004b]. More on the Russell protocol can be found in the next section.
Dr Sam Kunin, in Los Angeles, points out, however, that “the bell techniques leave too much inner skin. Besides the inherent problems of this method with later adhesions and buried penis, allows for possible migration of the bell down the shaft, with ensuing potential damage to the penile skin.” A Nigerian study also noted that incorrect technique can lead to proximal migration of the Plastibell in neonatal boys [Bode et al., 2009]. Correct training in this method is thus essential.
An Iranian study, involving 7,510 term neonates, found that Plastibell circumcision incorporating thermal cautery of the frenulum reduced bleeding (0.4% versus 0.05%), but led to greater urinary retention (0.03% versus 0.9%) [Kazem et al., 2009].
A study in Pakistan found that for babies under 3 months of age, the time taken for the Plastibell to fall off was 8.7 days [Samad et al., 2009]. This increased gradually to 16.8 days for children over 5 years.
Gomco clamp method:
First of all, a dorsal slit is made in the foreskin and the foreskin is separated from the glans. The bell of the Gomco clamp is then placed over the glans, and the foreskin is pulled over the bell. The base of the Gomco clamp is placed over the bell, and the Gomco clamp's arm is fitted. After the surgeon confirms correct fitting and placement (and the amount of foreskin to be excised), the nut on the Gomco clamp is tightened, causing the clamping of nerves and blood flow to the foreskin. The Gomco clamp is left in place for about 5 minutes to allow clotting of blood to occur, then the foreskin is dissected off using a scalpel. The Gomco's base and bell are then removed, and the penis is bandaged. It is a fairly bloodless circumcision technique. The circumcision is relatively quick compared to the Plastibell. It was the most popular method for circumcisions between 1950 and 1980 and is still common today, especially in the USA. There are also Gomco methods for adults. A training video of a neonatal GOMCO circumcision using dorsal penile nerve block and a sucrose pactifier, conducted by Dr Richard Green, Stanford University School of Medicine is available at http://newborns.stanford.edu/Gomco.html
Mogen clamp method:
Firstly adhesion between glans and foreskin are divided and a hemostat is placed along the dorsal midline with its tip about 3 mm short of the corona before being locked into place. The Mogen clamp is opened fully. A key step in Mogen circumcision is the safe placement of the clamp. To push the glans out of the way, the surgeon's thumb and index finger pinch the foreskin below the dorsal hemostat. The Mogen clamp is then slid across the foreskin from dorsal to ventral following along the same angle as the corona. The hollow side of the clamp faces the glans. Before locking the clamp shut, the glans is manipulated to be sure it is free of the clamp’s jaw. If it is, the clamp is locked. Once locked the foreskin is excised flush with the flat surface of the clamp with a 10 inch blade scalpel. The clamp is left on for a few moments to ensure hemotosis. It is then unlocked and removed. The crush line covers the glans line fully with penile shaft skin. The glans is liberated by thumb-traction at the 3 and 4 o'clock positions that pull the crush line apart.
Disposable clamp:
A plastic clamp (SmartClampCircumcisonDevice; SCD, Hengelo, The Netherlands) has been developed [Aldemir et al., 2007]. This fits on the penis much as the others do. After 4 days the connection between its inner tube and casing is cut and removed. The inner tube is then left to fall off spontaneously in time. Median operative time is 8 min, compared with 18 min for conventional dissection, and cosmetic result, judged blinded by a urologist, was better [Aldemir et al., 2007]. Parents’ satisfaction scores were the same.
The “Shenghuan Disposable Minimally Invasive Circumcision Anastomosis Device” developed in China involves minimal tissue manipulation and is said to give a simpler, quicker and safer circumcision than conventional techniques [Peng et al., 2008]. It was tested on 1,200 patients aged 5-95 years. Operating time was 2.5-3.5 min, after which it is worn for a week, with no incidents of device dislocation or damage to the frenulum. Oral diethylstilbestrol (2 mg/night) was used to prevent nocturnal erections. In 96.3% the incision healed, leaving minimal inner foreskin, with no scarring and good cosmetic results. Antibiotics were not used, and only 0.67% got an infection. After removal of the device 0.58% had some minimal bleeding around the incision and 2.4% had wound dehiscence of the incision caused by nocturnal erection, but this could be prevented by continuation of diethylstilbestrol for 3 days. It was treated by simply closing the incised rim with a butterfly adhesive plaster, followed by topical disinfectant; no stitches were required. Patients reported less pain than occurs for conventional methods.
A standardized surgical protocol has been established for the Shang ring and evaluation in 328 adult males showed an operating time of 4.7 ± 1.3 minutes, pain scores of 0.2 ± 0.6 during the surgery, 1.6 ± 1.0 24 hours postoperatively, 1.7 ± 1.1 24 hours prior to ring removal, and 2.7 ± 1.4 during ring removal [Cheng et al., 2009]. Complications included infection in 0.6%, bleeding in 0.6% and wound dehiscence in 0.6%; none of the latter required suturing. Penile edema occurred in 4.9%. The time for complete wound healing was 20.3 ± 6.7 days. Satisfaction was 99.7%.
Another disposable device is the AccuCirc (Clinical Innovations, Salt Lake City, Utah; www.clinicalinnovations.com; accucirc@clinicalinnovations.com). It uses two innovative components – a Foreskin Probe/Shielding Ring that ensures the glans is protected and the foreskin is properly aligned, and a Single-Action Clamp that ensures adequate hemostasis and the precise delivery of the protected, circular blade. These work together to protect the infant from injury. This device simplifies the circumcision procedure and eliminates the need for a dorsal slit, as well as removing potential for mismatching of parts. It comes in a self-contained kit. This is completely disposable and no part is retained on the infant.
A safe, simple, easy to use disposable plastic device advocated by the Turkish Professional Circumcisers Association is “Alisklamp” [www.alisklamp.com]. It can be used for infants through to adults, and comes in different sizes.
Tara Klamp:
A small randomized controlled trial in men of the Tara Klamp versus the forceps-guided method found adverse events in 37% versus 3%, respectively, so providing compelling evidence that cautions against use of the Tara Klamp [Lagarde et al., 2009].
General comments:
The various devices serve to protect the penis when excising the prepuce. The type of clamp used affects the time taken for the procedure, being on average 81 seconds for the Mogen clamp and 209 seconds for the Gomco clamp [Kurtis et al., 1999]. In a head-to-head trial of length of procedure the Mogen took 12 minutes, compared with 20 minutes for the Plastibell [Taeusch et al., 2002]. Although simpler to use and more pain-free than the other two [Kurtis et al., 1999; Kaufman et al., 2002; Taeusch et al., 2002], the Mogen removes less foreskin. The Gomco is the oldest, having been invented in 1935, and is the most refined instrument [Wan, 2002]. Since some of these more elaborate methods can take up to 30 min to perform they therefore expose the baby to a greater period of discomfort. In contrast, a circumcision can be completed in 15-30 seconds by a competent practitioner using methods that are part of traditional cultures.
Interestingly, strict sterile conditions were reported not to be necessary to prevent infection in ritual neonatal circumcision in Israel [Naimer & Trattner, 2000].
Rather than tightly strapping the baby down, swaddling and a pacifier has been suggested [Herschel et al., 1998; Howard et al., 1998; Howard et al., 1999]. A special padded, “physiological” restraint chair has, moreover, been devised and shown to reduce distress scores by more than 50% [Stang et al., 1997]. Exposure to a familiar odor (their mother’s milk or vanilla) reduces distress after common painful procedures in newborns [Goubet et al., 2003; Rattaz et al., 2005; Goubet et al., 2007].
Dr Tom Wiswell and other experts strongly advocate the neonatal period as being the best time to perform circumcision, pointing out that the child will not need ligatures (owing to the thinness of the foreskin [Schoen, 2005c]) or general anesthesia, nor additional hospitalization [Wiswell & Geschke, 1989; Wiswell & Hachey, 1993; Wiswell, 1995; Wiswell, 1997a; Wiswell, 2000]. Wiswell pointed out (personal email communication in Apr 2009) that “starting in the 1970s there was a movement away from delivery room circumcisions at minutes of life until several hours to several days of life. This was mainly because of the recognition of the transition period to extrauterine life that babies go through. “Stresses” can have an adverse effect on this process, particularly on the heart and lungs. In an otherwise healthy infant, though, there is no need to delay until 2 weeks of age.”
Without an anesthetic the child experiences pain, and pain is also present for from a few up to a maximum of 12-24 hours afterwards. The child does not, however, have any long-term memory of having had a circumcision performed. A greater responsiveness to subsequent injection for routine immunization may suggest, however, that the baby could remember for a short time [Taddio et al., 1997b]. Local anesthesia is therefore advocated (see below). Healing is rapid in infancy [Schoen, 2005c], complication rate is very low (0.2%), and cost is about one-tenth (discussed later).
Older children
Circumcision is more traumatic, disruptive and expensive for older boys [Schoen, 2007e]. For children aged 4 months to 15 years some authorities advocate a general anesthetic. Others strongly disagree, saying that since a general anesthetic carries a small risk, a local anesthetic, often with a mild sedative, should be used for all children [Schoen, 2007e].
It should also be noted that ligatures (sutures/stitches) are usually needed for older children, although use of a tissue glue [Subramaniam & Jacobsen, 2004; Ozkan et al., 2005; Lane et al., 2009b] or a synthetic tissue adhesive (Dermabond) [Elmore et al., 2007] have proven to be effective alternatives. The latter also reduce operating time and give a better cosmetic appearance [Ozkan et al., 2005; Elmore et al., 2007].
Excellent cosmetic results were reported for all of 346 patients aged 14 to 38 months using electro-surgery, which presents a bloodless operative field [Peters & Kass, 1997]. Metal of any kind (such as the Gomco clamp) has to of course be avoided in this procedure.
Gentle tissue dissection with simultaneous hemostasis was achieved using an ultrasound dissection scalpel for circumcision [Fette et al., 2000]. A randomized trial found that a bipolar diathermy scissors circumcision technique led to less blood loss (0.2 versus 2.1 ml), shorter operating time (11 versus 19 min) and lower early and late postoperative morbidity as compared with a standard freehand scalpel procedure [Méndez-Gallart et al., 2009].
Circumcision later obviously requires a separate (occasionally overnight) visit to hospital. Healing is slower than in newborns, and rate of complications is greater, but still low (ranging from less than 1% to approx. 3%). The incidence of penile adhesions decreases with age, but at any age they often resolve spontaneously [Ponsky et al., 2000]. Pain sometimes can last for days afterwards and those older than 1 to 2 years may remember. Cost is also much greater than for neonatal circumcision.
For boys with hemophilia, special pre-operative treatment is required. A satisfactory outcome can also be achieved with a specialized cost-effective device [Karaman et al., 2004].
Adults
Much of what is stated above for older boys applies to adults. Stitches (or tissue glue) are required and in adults circumcision is more expensive. Cost can be reduced by having it performed on an outpatient basis. A local anesthetic is all that is needed (so reducing anesthetists charges which can be quite high for a general anesthetic). Best results are obtained with the sleeve-resection technique, described in a series of diagrams with technical details by Elder [2007b]. This method takes longer and for this reason many surgeons will insist on a general anesthetic being used if this method is chosen.
Pain can last for up to a week or so afterwards, during which time absence from work may be required. Some, however. report no pain, just minor discomfort from the stitches. Vasectomy in men circumcised previously as adults (and who can thus attest to the difference) is said to be much more painful. Interestingly, genital surgery in women often involves a course of topical estrogen in advance to increase thickening, cornification and keratinization of the vaginal epithelium [Short, 2006]. This helps surgical outcome and has led to the suggestion that similar pre-treatment be carried out prior to male circumcision.
The WHO have produced a manual for circumcision of men under local anesthesia [WHO, 2006].
Devices
For an extensive review of the instrumentation used for circumcision of males of varying ages refer to a popular review [Morris & Eley, 2011].
Conclusion:
For an extensive review of the instrumentation used for circumcision of males of varying ages refer to a popular review [Morris & Eley, 2011].
Thus when considering when is the best time, it would appear that circumcision in the newborn period is safe and technically easy. It is also more convenient, is not remembered by the male, and is much cheaper, as well as providing the maximum lifetime benefit. See later section on cost-benefit and specific section on why circumcision should not be delayed, which provides an itemized list of reasons.



